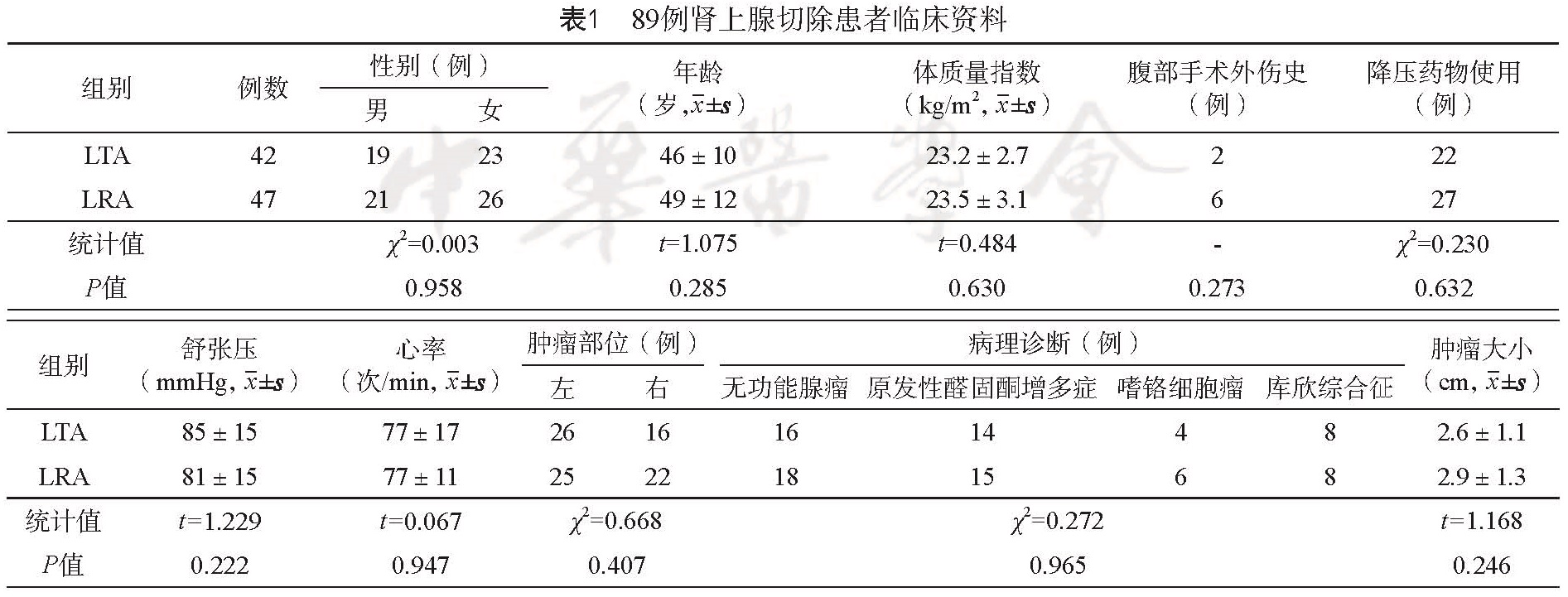
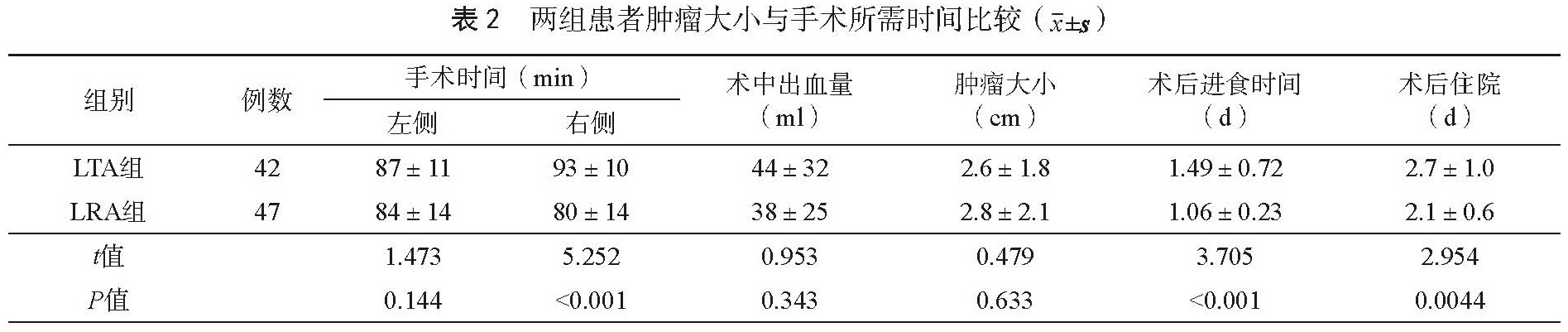
目的 比较经腹腔肾上腺切除术(LTA)与腹膜后肾上腺切除术(LRA)两种不同入路腹腔镜肾上腺切除术的临床疗效。方法 回顾性分析2012年1月至2016年12月89例在我院泌尿外科施行腹腔镜肾上腺肿瘤切除术患者的临床资料,对两种不同入路肾上腺切除术患者手术时间、术中出血量、肿瘤大小、术后进食时间和平均住院时间进行比较分析。结果 89例患者中采用LTA入路 42例,LRA入路 47例。两组患者性别、年龄、腹部手术、外伤史、口服降压药物史、术前血压、心率、肿瘤部位、临床诊断及肿瘤大小差异均无统计学意义(P>0.05)。LRA组平均手术时间短于LTA[(78±17)mins vs (90±21) mins, P=0.0047]。而 LRA入路的右侧肾上腺切除平均所需时间较LTA入路更短 [(80±14)vs(93±10),P<0.001],两组左侧肾上腺切除所需时间差异无统计学意义 [(84±14) vs (87±11),P=0.144]。两组术中出血量 [(38±25)ml vs (44±32)ml,P=0.343]、肿瘤大小均无统计学差异(P>0.05),而术后进食时间及住院天数差异有统计学意义。结论 LTA和 LRA入路肾上腺肿瘤切除均可达到安全、满意的疗效。采用 LRA术式平均手术时间短于 LTA术式,术后患者恢复较 LTA组快。
Objective To compare the clinical effect of two approaches to laparoscopic adrenalectomy: laparoscopic transperitoneal approach (LTA) and laparoscopic retroperitoneal adrenalectomy (LRA). Methods The clinical data of 89 cases underwent laparoscopic adrenalectomy from January 2012 to December 2016 in our department were retrospectively analyzed. The mean operative time, perioperative blood loss, tumor size, first oral intake and postoperative hospital stay were compared and analyzed between LTA and LRA groups Results LTA was performed in 42 patients and LRA in 47 patients. There was no significant difference in gender, age, history of abdominal surgery, antihypertensive medication history, preoperative blood pressure, preoperative heart rate, tumor location, clinical diagnosis and tumor size between LTAand LRAgroup (P>0.05). The mean operating time in LRA group was shorter than that in LTA [(78±17) min vs (90±21) min, P=0.0047)], especially for patients in the LRA group underwent right adrenalectomy [(80±14) min vs (93±10) min, P<0.001)]. However, those underwent left adrenalectomy had no significant difference between LRA group and LTA group [(84± 14) min vs (87±11) min, P=0.144]. There was no significant difference in blood loss[(38±25) ml vs (44± 32) ml, P=0.343] and tumor size. While there were significant differences in the average hospitalization and first oral intake between LRA and LTA (P<0.05). Conclusion LTA and LRA can be safe and effective. The mean operating time in PRA group was shorter than in LTA group, and the postoperative recovery in PRA was faster than that of the LTA group.